Restructure Your Business to Provide Better Social Impact, Increase Revenue, and Get Your Startup Running Like Clockwork… Without You!
Do you know how to open the gateway to profitability with a bootstrap budget?
Give me a call to learn how.
As Featured In







Join Sabrina's Inner Circle of Healthcare Disruptors
As the saying goes, it's not what you know, it's who you know.
Love podcasts?
Subscribe to the Provider’s Edge podcast to learn and grow from experts
who have been in your shoes!
The Provider’s Edge podcast and TV shows feature medical, dental, and holistic practice owners, executives, and innovators to discuss how to create more impact, more profit, and more freedom while running their businesses.
Sabrina’s guests share stories about how they are growing their practices and discuss the best strategies in order to encourage other leaders like them to excel in their practice.
The Provider’s Edge audience is major. This show is rated in the top 5% of podcasts globally, with 30k+ downloads, so that means a lot of visibility for her guests and instant connection with thousands of their fellow practitioners. She’s giving practitioners a forum to build authority in their field and allow their patients to see their authentic side as well.
Healthcare leaders, you have a lot on your plate and too much to figure out all at once.
On top of caring for your patients, managing your staff, and keeping your books straight, it's no wonder that so many healthcare leaders have a hard time keeping up with the demand of their businesses.
When you can't catch a break in the present, it is challenging to see the way forward into the future.
But it doesn’t have to be this way. Take it from me.
You just need to understand how to open the gateway to profitability by gaining visibility and credibility with the right circles. I can show you how!

Healthcare leaders, you have a lot on your plate and too much to figure out all at once.
On top of caring for your patients, managing your staff, and keeping your books straight, it's no wonder that so many healthcare leaders have a hard time keeping up with the demand of their private practice.
When you can't catch a break in the present, it is challenging to see the way forward into the future.
But it doesn’t have to be this way. Take it from me.

Hi, I'm Sabrina
I’ve been in your shoes…
After working 80 hours a week as a cardiothoracic surgery physician associate, my workload took a toll on my personal and professional life. Even though I had achieved what most people considered “success”, it wasn’t the life I wanted to live. That was when I realized something needed to change. I took a deep dive into performance sciences and positive intelligence and made some amazing discoveries I applied directly. As a result, I decreased my clinical work hours by 30% and increased my income by 50%. I was so inspired by my experience, I now offer consulting services to help other healthcare leaders achieve the same results: work less, provide better care, and generate more revenue AT THE SAME TIME as I did. I get the best of both worlds and live the life of my dreams!
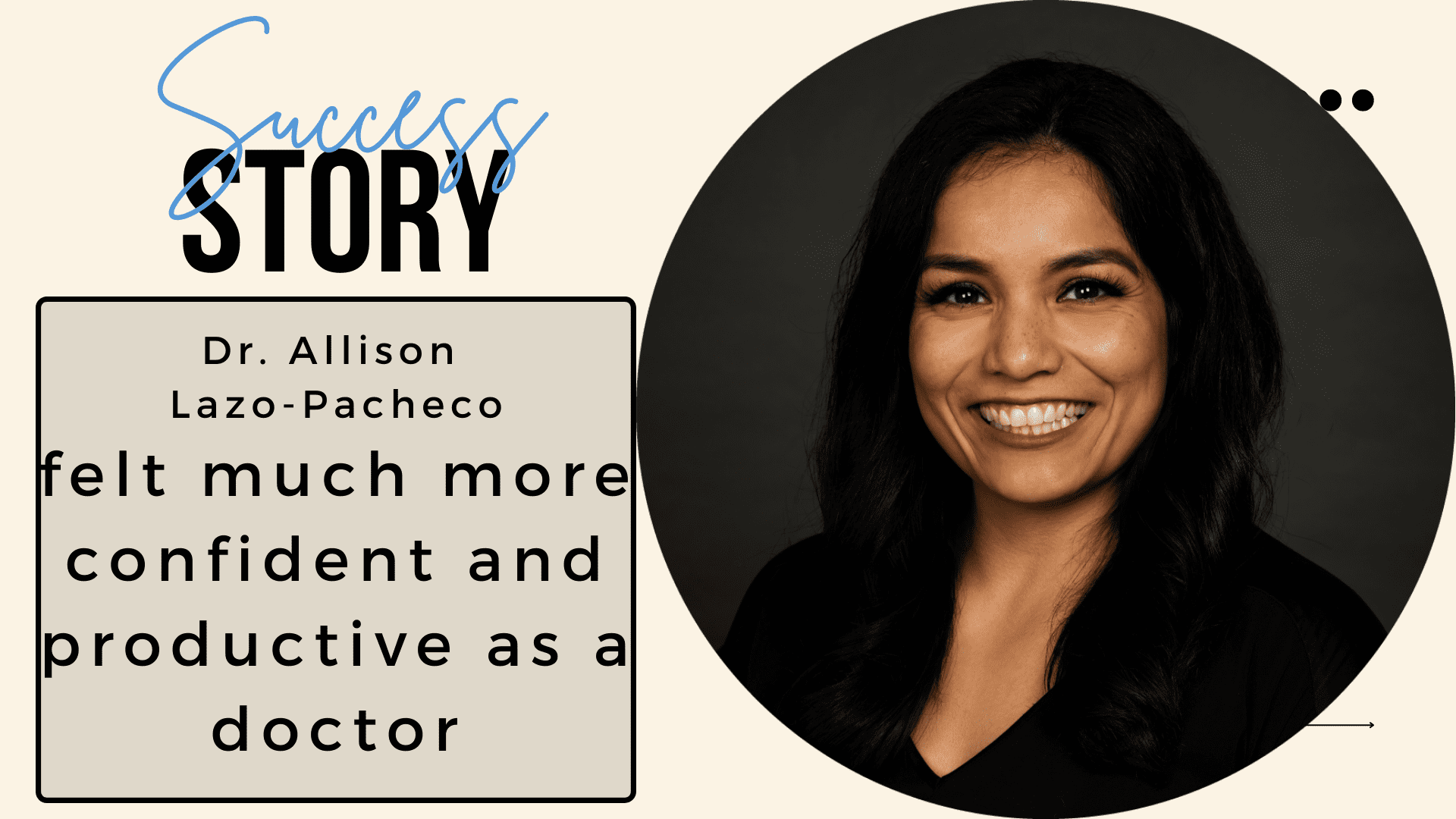
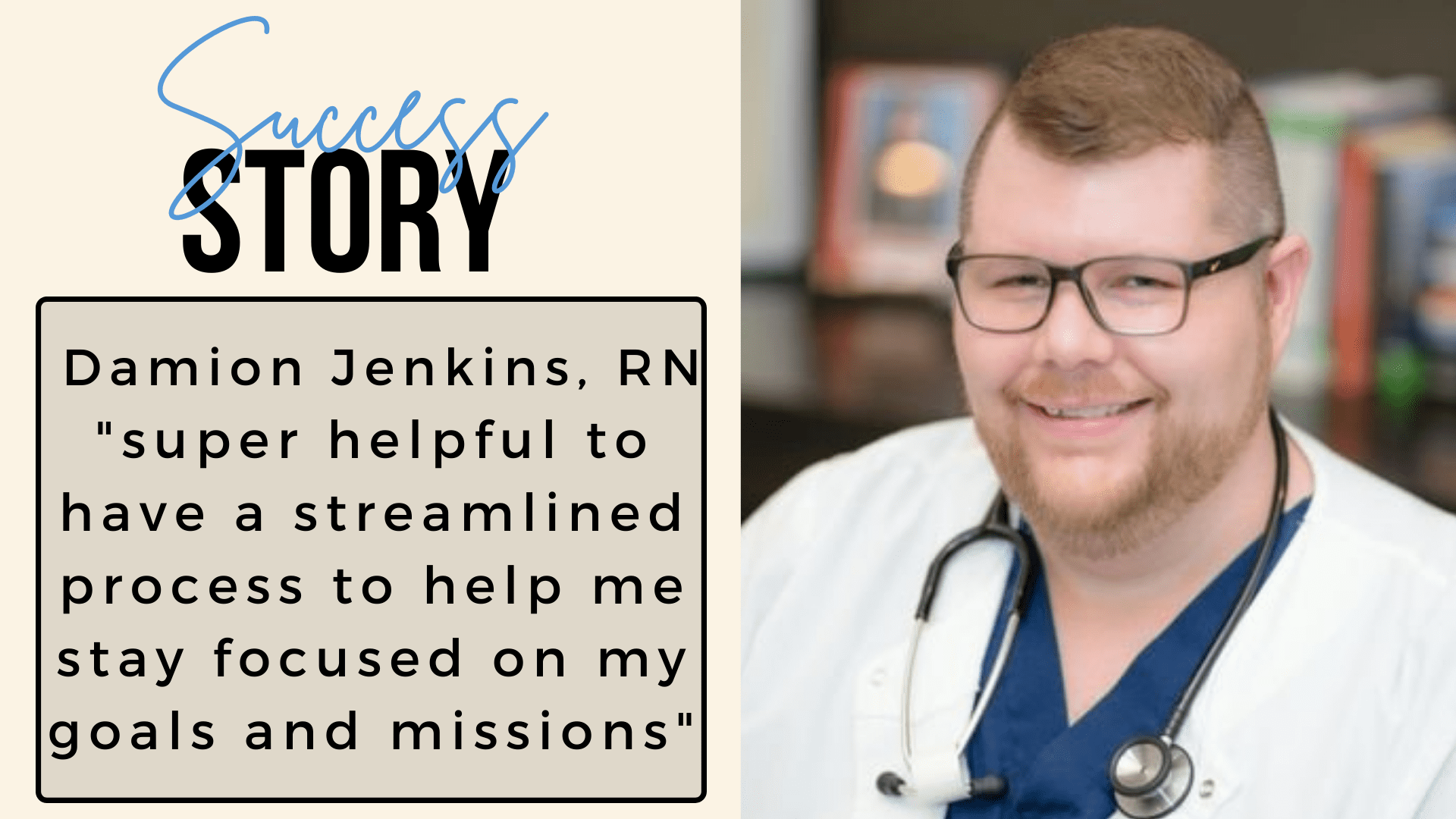
By working with me, my clients have been able to:
• Stop worrying about where their next ads budget will come from
• Move steadily forward with more profit margins
• Gain a day back per week for themselves
So if you're feeling overwhelmed and don’t know what to do, don’t fret. There is hope.
…and I’m here to help! Let’s have a conversation to help you reclaim your freedom and expand your business with clear and focused strategies.
The Solutions
Learn how to create Millionaire Marketing on a bootstrap budget by leveraging key relationships and creating a high-net-worth network to share your mission, your messages, and your solutions in the healthcare space.
Find out the true health of your business with this in-depth assessment to ensure everything is working at tip-top shape!
Sharpen your executive skills and knowledge to grow your private practice, relieve decision fatigue, and gain one more day in your week.
Get unlimited sessions and support with Sabrina to uplevel your success, on your schedule!
Connect With Sabrina Here:
Copyright © 2022 Sabrina Runbeck LLC | Credits
Powered by Sabrina Runbeck LLC.